Complete Guide to Next-Generation Digestive Endoscopy Equipment (2026)
admin
January 29, 2026
Introduction
Digestive endoscopy has undergone significant evolution in recent years. Modern systems are no longer limited to basic visualization of the gastrointestinal tract; they have become advanced diagnostic platforms incorporating cutting-edge imaging technologies, image enhancement features, and strategic considerations that directly impact diagnostic accuracy, procedural safety, and return on investment (ROI) for clinics and hospitals.
In this complete guide, you will understand what defines next-generation digestive endoscopy equipment, learn about the systems currently in highest demand, compare technologies, and discover how to choose the most suitable equipment for your clinical and financial profile.
What Defines Next-Generation Digestive Endoscopy Equipment?
A common misconception is that “next-generation” refers only to the year of manufacture. In practice, a modern endoscopy system is defined by a combination of technical performance, clinical capability, and long-term reliability, including:
High image resolution (HD, Full HD, or higher)
Advanced image enhancement technologies
Stable and efficient light sources
Compatibility with modern endoscopes
Reliability for high-volume clinical use
Ease of maintenance and availability of spare parts
Upgrade and scalability potential
These factors directly influence diagnostic accuracy, procedural safety, workflow efficiency, and operational costs over the lifetime of the equipment.
Main Components of a Modern Digestive Endoscopy System
Image Processor
The image processor is the core of any endoscopy system. It converts signals captured by the endoscope into diagnostic-quality images displayed on the monitor.
Next-generation processors offer:
Improved contrast and sharpness
Advanced color processing
Reduced image noise
Integrated image enhancement technologies
Examples of modern platforms widely used in the market include systems such as Fujifilm VP-7000, Olympus CV-190, Olympus EVIS X1, Pentax EPK-i, and Pentax Imagina.
Light Source
Proper illumination is critical for safe and accurate examinations. Modern systems increasingly rely on LED light sources, which provide:
Longer operational lifespan
Stable and uniform illumination
Lower heat generation
Reduced maintenance and replacement costs
LED technology has largely replaced xenon lamps in newer platforms.
Endoscopes (Scopes)
The final image quality depends heavily on the endoscope itself. Market trends favor high-resolution scopes with improved ergonomics, durability, and compatibility with advanced platforms.
Fujifilm’s 760 series scopes are widely recognized for:
Excellent image quality
Robust construction
Compatibility with modern processors
Strong acceptance in the refurbished equipment market
Image Enhancement Technologies: Clinical Impact
One of the most important advances in modern digestive endoscopy is the development of image enhancement technologies, which significantly improve visualization of mucosal patterns and vascular structures.
Key technologies include:
Narrow Band Imaging (NBI) – enhances vascular patterns
Blue Light Imaging (BLI) – improves mucosal detail
Linked Color Imaging (LCI) – increases color contrast
i-Scan – digital surface and pattern enhancement
These technologies support early lesion detection, better characterization, and increased diagnostic confidence.
Digestive Endoscopy Systems in High Demand in 2026
Among the most sought-after systems currently on the market are:
Fujifilm VP-7000 / BL-7000 – advanced platform compatible with 760 series scopes
Fujifilm EP-600 – modern system with strong cost-benefit balance
Olympus CV-190 / CLV-190 – widely adopted and well-established platform
Olympus EVIS X1 – flagship system with advanced imaging capabilities
Pentax EPK-i 7010 and 5010 – reliable and robust platforms
Pentax Imagina – next-generation evolution of Pentax imaging systems
These systems are commonly selected by clinics and hospitals seeking technological modernization without compromising reliability.
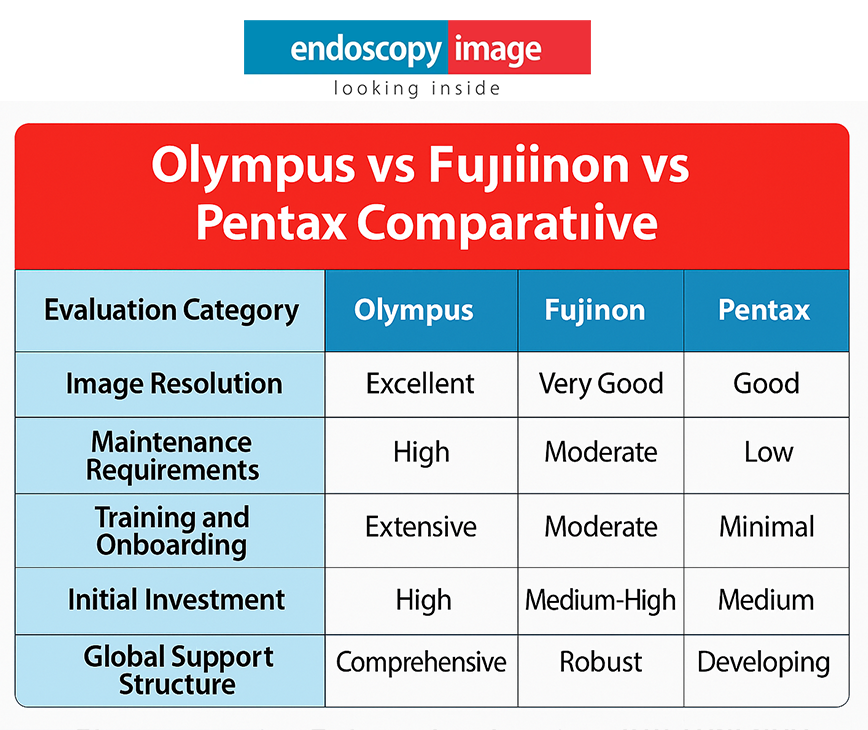
Practical Comparisons: What Buyers Want to Know
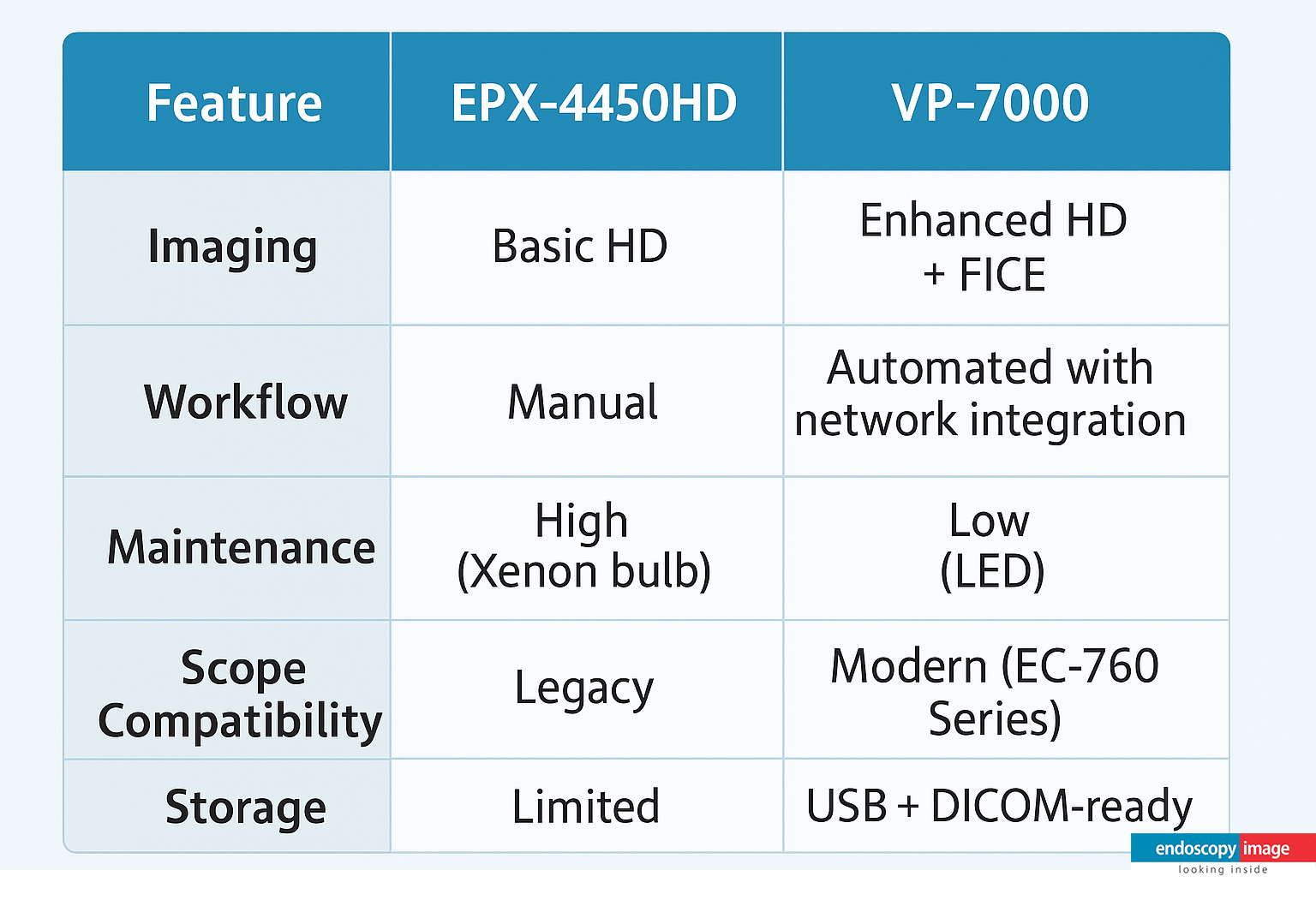
Fujifilm VP-7000 vs Olympus CV-190
VP-7000 focuses on advanced image enhancement technologies (BLI and LCI) and compatibility with modern scopes.
CV-190 is known for its large installed base, reliability, and ease of maintenance.
Both platforms are excellent choices; the ideal option depends on clinical goals and investment strategy.
Pentax Imagina vs Pentax EPK-i 7010
EPK-i 7010 remains a trusted and widely used system.
Imagina represents the technological evolution, offering improved image processing and performance.
Clinics aiming for long-term technological advancement often favor the Imagina platform.
Endoscopic Ultrasound (EUS): A Specialized Segment
Endoscopic ultrasound combines endoscopy and ultrasonography, requiring highly specialized and reliable systems.
Commonly used EUS processors include:
EU-ME1
EU-ME2
SU-1
Systems such as Noblus, paired with EUS scopes like EG-3870TK and EG-3870URK, are well known in the EUS segment for specific clinical applications.
How to Choose the Right Endoscopy System
Before investing in a next-generation system, it is essential to evaluate:
Monthly procedure volume
Types of examinations and interventions performed
Compatibility with existing scopes
Maintenance and service costs
Spare parts availability
Upgrade potential
Budget and expected ROI
The best system is not necessarily the most expensive, but the one that best fits your clinical workflow and operational reality.
New, Used, or Refurbished Equipment: When Does It Make Sense?
Next-generation systems are also available as used or refurbished equipment. When properly inspected and supported by warranty and technical service, refurbished systems can offer:
Access to advanced technology
Lower upfront investment
Reliable clinical performance
This option is particularly attractive for clinics seeking modernization with controlled capital expenditure.
FAQ: Next-Generation Digestive Endoscopy Equipment
➡️ This depends on evaluation criteria. Platforms such as VP-7000, EVIS X1, and Pentax Imagina are among the most advanced currently available.
➡️ Yes, provided the system has verified origin, thorough technical inspection, warranty, and ongoing support.
➡️ Yes. These systems offer excellent image quality, durability, and strong resale value.
➡️ Prioritize based on your biggest bottleneck. In many upgrades, the image processor delivers the most immediate improvement in image quality and enhancement features, but scopes are critical because they ultimately determine what the system can capture. A modern LED light source improves consistency and reduces maintenance, but it usually comes after confirming processor/scope compatibility.
➡️ Confirm verified origin and a documented inspection process, check compatibility between processor/light source/scopes, ask about included accessories, warranty terms, service turnaround time, and spare parts availability. Also evaluate total cost of ownership (maintenance, parts, consumables) rather than purchase price alone.
Topics that might interest you:
Blog & Articles
What Makes the Olympus EVIS X1 One of the Most Advanced Endoscopy Systems on the Market
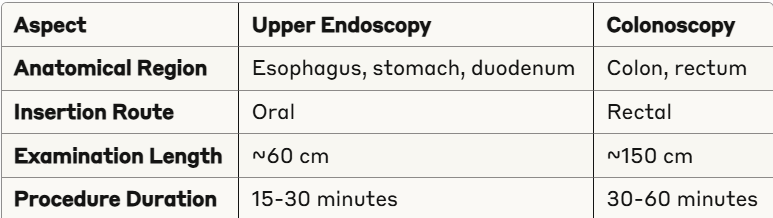
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
Complete Guide to Next-Generation Digestive Endoscopy Equipment (2026)
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
Endoscopy Equipment in Mexico and Latin America: Your Complete 2025 Buying Guide
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
Endoscopy and Colonoscopy: The Complete Guide to Understanding Procedure Differences in 2025
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..