What Makes the Olympus EVIS X1 One of the Most Advanced Endoscopy Systems on the Market
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
+1 (786) 681-5247
admin
September 10, 2025

If you’ve ever found yourself or your patients confused about the differences between endoscopy and colonoscopy, you’re not alone. This confusion affects thousands of medical professionals and patients daily, leading to miscommunication and suboptimal patient care.
The reality is that colonoscopy is actually a type of endoscopy – but this technical distinction often gets lost in clinical practice. While “endoscopy” typically refers to upper gastrointestinal examination, the broader definition encompasses any procedure using an endoscope to visualize internal organs.
In this comprehensive guide, we’ll break down the critical differences between these procedures, explore the latest equipment innovations from leading manufacturers like Olympus, Fujifilm, and Pentax, and provide you with actionable insights to optimize patient outcomes and clinical efficiency.
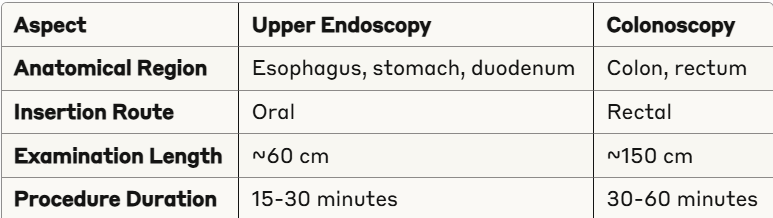
Upper endoscopy, also known as esophagogastroduodenoscopy (EGD), involves the examination of the upper digestive tract using a flexible endoscope. This procedure allows direct visualization of the esophagus, stomach, and duodenum (first part of the small intestine) through oral insertion.
Upper endoscopy serves multiple diagnostic and therapeutic purposes:
Modern upper endoscopes feature advanced imaging capabilities with 4K resolution and narrow-band imaging (NBI) technology. Leading manufacturers offer:
Colonoscopy involves the examination of the large intestine (colon) and rectum using a flexible colonoscope inserted through the rectum. This procedure can visualize the entire colon, making it the gold standard for colorectal cancer screening and polyp detection.
Recent guidelines have transformed colonoscopy recommendations. The U.S. Preventive Services Task Force now recommends that adults begin colorectal cancer screening at age 45 (previously 50) for average-risk individuals. This change reflects the rising incidence of colorectal cancer in younger populations.
For adults aged 76-85, screening recommendations become selective, based on individual health status and patient preferences.
Colonoscopy is indicated for:
Both procedures typically use moderate sedation (conscious sedation), but colonoscopy often requires deeper sedation due to:
Recovery times are generally similar (30-60 minutes), though colonoscopy patients may experience more post-procedure bloating due to CO2 insufflation.
The integration of artificial intelligence in endoscopy and colonoscopy has revolutionized polyp detection rates. Key systems include:
The global endoscopy equipment market reached $29.5 billion in 2024 and is projected to grow at 6.9% annually through 2034. This growth is driven by:
Choose Upper Endoscopy for:
Choose Colonoscopy for:
In certain clinical scenarios, same-day upper endoscopy and colonoscopy may be appropriate:
This approach offers cost savings and improved patient convenience while maintaining safety profiles.
➡️ The primary difference lies in the anatomical area examined. Upper endoscopy (EGD) examines the esophagus, stomach, and duodenum through oral insertion, while colonoscopy examines the colon and rectum through rectal insertion. Technically, colonoscopy is a type of endoscopy, but in clinical practice, "endoscopy" typically refers to upper GI examination.
➡️ Yes, same-day upper endoscopy and colonoscopy can be safely performed when clinically indicated, such as for unexplained iron-deficiency anemia or obscure GI bleeding evaluation. This approach offers patient convenience and cost savings while maintaining safety standards. The procedures can share the same sedation event, reducing overall recovery time.
➡️ The U.S. Preventive Services Task Force lowered the recommended screening age to 45 in response to rising colorectal cancer rates in younger adults. Studies show that starting screening at 45 can prevent more cancers and save more lives through earlier detection of precancerous polyps and early-stage cancers in the 45-49 age group.
➡️ A transnasal endoscope is recommended for patients who cannot tolerate traditional upper GI endoscopy. It offers a more comfortable, less invasive approach, often without sedation, making it ideal for sensitive or anxious patients.
➡️ Capsule endoscopy offers a painless, non-invasive way to visualize the small intestine. Unlike traditional scopes, it can reach areas that are otherwise difficult to access, making it especially valuable for detecting obscure gastrointestinal bleeding or Crohn’s disease.
Understanding the distinct differences between endoscopy and colonoscopy is crucial for delivering optimal patient care in 2025. While both procedures share the common goal of visualizing internal anatomy for diagnostic and therapeutic purposes, their specific applications, patient preparation requirements, and clinical outcomes differ significantly.
The recent shift to begin colonoscopy screening at age 45, combined with advancing AI technology and improved equipment capabilities, presents new opportunities to enhance patient outcomes and clinical efficiency. By staying current with these developments and maintaining clear communication with patients about procedural differences, healthcare providers can optimize screening compliance and diagnostic accuracy.
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
Discover the key differences between endoscopy and colonoscopy procedures. Expert guide for medical..
Deprecated: File Theme without comments.php is deprecated since version 3.0.0 with no alternative available. Please include a comments.php template in your theme. in /home/endoscop/public_html/wp-includes/functions.php on line 6131